Abstract
BACKGROUND: An important progress has been made in understanding the pathophysiology of lower risk MDS in recent years. This progress has been more relevant in some specific subtypes such as del(5q) MDS or MDS with RS (>15% RS in BM or >5% RS + SF3B1 mut). In fact, for the latter subtype, in-depth knowledge of its pathophysiology has led to the recent development of new therapeutic strategies (luspatercept). In this regard, new WHO 2017 classification identify in the lower risk MDS setting 2 categories of patients with different clinical and biological features: those without RS (<5%) and those with RS, involving 2 subgroup of patients (those with >15% of RS and those with <15% and >5% of RS and the presence of SF3B1 mutations. Unfortunately, no clear data regarding disease characteristics and outcome have been analyzed to identify these 3 new subgroups of patients, are those with 5-15RS really like those with >15RS? Therefore, improving knowledge in real life setting of these subgroups of patients will lead to optimize the therapeutic management and the potential development of new therapeutic strategies.
AIMS: Our aim was to describe baseline clinical characteristics and their implication in overall survival (OS), progression free survival (PFS) and transfusion free survival (TfFS) among LR-MDS according to the presence of RS. We compare 3 sub-categories within the current WHO classification.
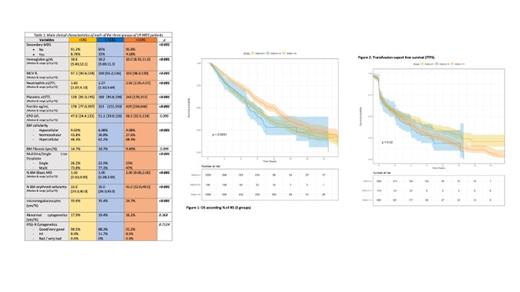
METHODS: A retrospective study from the Spanish MDS registry was performed in which patients diagnosed with low-risk MDS (Very low to int risk IPSS-R) were selected. MDS with excess of blasts, del(5q) and/or MDS/MPS were excluded. Finally, 2250 patients were selected which were classified according to the percentage of RS into three groups: 1) patients without RS (defined as less than 5% RS, <5RS) (n=1256), 2) patients with ≥5% and < 15% RS (5-15RS) (n=196) and 3) patients with ≥ 15% RS(>15RS) (n=1098). Descriptive analysis and survival estimation was done according to classical definitions (OS, PFS). Transfusion free survival (TfS) was defined from diagnosis to the development of transfusion dependency.
RESULTS: In <5RS group, median age at diagnosis was 75.0 years [p25-p75 68.0;81.0] and 61% patients were male. Main clinical characteristics are summarized in table 1. Patients with <5RS had higher hemoglobin level than the others with also a smaller MCV. However, neutrophils and platelets counts were lower in <5RS subgroup compared to 5-15RS and >15RS patients. Ferritin level at diagnosis was also lower for <5RS. Less than 50% of <5RS patients had an hypercellular BM as opposed to almost 70% in >15RS group and as expected, erythroid cellularity was lower in <5RS as compared to >15RS. Regarding single or multiline dysplasia, patients with <5RS and 5-15RS generally developed multiline dysplasia (74% and 77%, respectively) as compared to those with >15RS (47%). Median blast% was higher in patients with <5RS compared to the other groups. Moreover, the percentage of micromegakaryocytes (adverse prognosis) observed was higher in the group with <5RS and 5-15RS. No clear differences were observed according to cytogenetic abnormalities.
Median follow-up was 4.1 years. Interestingly, median OS and range (p25-p75) for <5RS pts was 5.67 yr (2.4-10.2), close similar to 5-15RS pts (4.93 yr 2.4-10.6) and inferior to >15RS pts (7.66 yr 3.7-12.3) p<0.0001 (Figure1). Progression to RAEB/AML was observed in 11.3%, 9.69% and 7.01% of patients in <5RS, 5-15RS and >15RS groups respectively (p=0.002).
In this sense, PFS for LR-MDS with <5RS was 5.1 yr (2.1-9.8), close similar to the 5-15RS group (4.77 yr (1.9-10.7)) and inferior to >15RS pts (7.01 yr (3.5-12.3) (p<0.0001). Contrary to OS/PFS, TfFS was favorable to the <5RS group (median 3.2 yr 0.1-10.4) as compared to 5-15RS (2.13 yr 0.1-6.6) and >15RS (2.4 yr 0.1-7.6) patients (Figure2, p=0.02).
SUMMARY: Clinical and biological characteristics of LR-MDS patients according to RS are different and impact on survival, disease evolution and need of treatment. Patients with 5-15RS are in an intermediate situation from <5RS and >15RS regarding clinical and biological variables and with poorer outcome than >15RS patients. A better understanding of these subgroups could help us to personalize therapeutic options in this heterogeneous subset of patients.
Sanz: Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees; Roche: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel, accommodations, and expenses; Amgen: Consultancy, Membership on an entity's Board of Directors or advisory committees; Boehringer Ingelheim: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel, accommodations, and expenses, Speakers Bureau; Gilead Sciences: Other: Travel, accommodations, and expenses; Helsinn Healthcare: Consultancy, Membership on an entity's Board of Directors or advisory committees; Abbvie: Consultancy, Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Travel, accommodations, and expenses, Research Funding. Tormo: Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Jazz Pharmaceuticals: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Pfizer: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Amgen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Astellas: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Valcárcel: Sanofi: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Pfizzer: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; MSD: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Jazz: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Jansen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Celgene/BMS: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Astellas: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Amgen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Sobi: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Takeda: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Diez-Campelo: BMS: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Takeda Oncology: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau.